Erectile dysfunction (ED) has long been managed with a one-size-fits-all mentality, dominated by the use of phosphodiesterase type 5 (PDE5) inhibitors such as sildenafil. While these agents revolutionized the field by providing a safe, effective, and convenient oral therapy, a growing body of evidence suggests that monotherapy often leaves many patients dissatisfied. Clinical realities—ranging from hypogonadism and diabetes to surgical sequelae of prostatectomy—demand a more nuanced approach.
Recent systematic reviews and meta-analyses, including a comprehensive evaluation of 44 clinical studies, demonstrate that combination therapy may represent the next frontier in ED management. By merging pharmacological, mechanical, and regenerative strategies, clinicians can move beyond symptomatic relief toward more robust, individualized outcomes.
Understanding the Limitations of Monotherapy
PDE5 inhibitors remain the cornerstone of first-line ED treatment. Their mechanism, enhancing nitric oxide (NO)–cGMP signaling to facilitate cavernosal smooth muscle relaxation, is elegant in its simplicity. Yet even with sildenafil, tadalafil, or vardenafil available, response rates vary widely. More than half of patients eventually report partial benefit, discontinuation, or complete dissatisfaction.
The reasons are multifactorial. Organic etiologies such as vascular disease, neurogenic injury, and hypogonadism reduce drug efficacy. Psychological barriers, medication side effects, and contraindications further limit adherence. For men post-radical prostatectomy, nerve damage and endothelial dysfunction significantly blunt PDE5 inhibitor efficacy. In diabetic populations, endothelial resistance compounds the challenge. Clearly, the celebrated blue pill is not an omnipotent solution.
This recognition sets the stage for exploring whether therapeutic synergies—pairing PDE5 inhibitors with adjunctive modalities—can rescue function where monotherapy falters.
Combination Therapy: A Systematic Evidence Base
The meta-analysis under discussion incorporated 44 studies involving nearly 4000 men, with a mean age of 56 years. Outcomes were evaluated using validated questionnaires such as the International Index of Erectile Function (IIEF). The pooled data demonstrated that combination therapy improved erectile function scores significantly more than PDE5 inhibitor monotherapy.
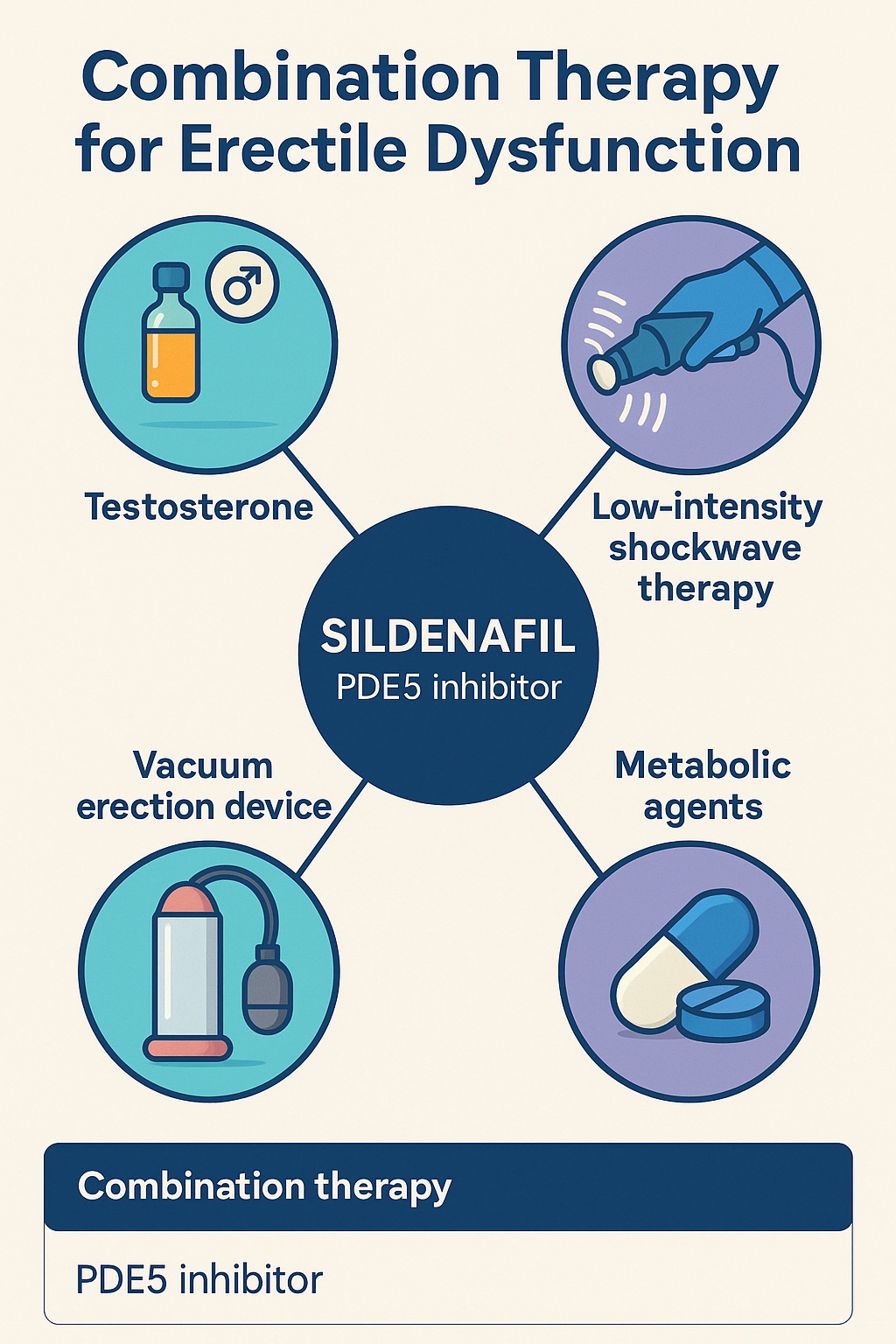
What is striking is not only the magnitude of improvement but also the diversity of strategies trialed. Adjuncts ranged from pharmacological agents like testosterone, metformin, folic acid, and angiotensin-converting enzyme inhibitors to mechanical methods such as vacuum devices and low-intensity extracorporeal shockwave therapy (Li-ESWT). Importantly, safety outcomes showed no significant increase in adverse events, reinforcing that enhanced efficacy did not come at the expense of tolerability.
This evidence underscores that ED is not a uniform disease but a syndrome with diverse pathophysiological roots. Combination strategies allow clinicians to target multiple mechanisms simultaneously, thereby tailoring therapy to individual patient needs.
Testosterone Supplementation: Restoring the Missing Link
One of the most consistent findings is the benefit of combining PDE5 inhibitors with testosterone replacement in hypogonadal men. Hypogonadism not only diminishes libido but also downregulates PDE5 expression and nitric oxide synthase activity, impairing drug response. Clinical trials demonstrated that adding testosterone patches, gels, or intramuscular injections to sildenafil or tadalafil yielded meaningful improvements in erectile scores.
Beyond erections, testosterone repletion addresses systemic consequences such as sarcopenia, anemia, and depressive symptoms. In this context, sildenafil becomes part of a broader restorative strategy rather than a symptomatic quick fix. Notably, improvements in erectile function did not require supraphysiologic dosing but rather restoration to normal ranges—an elegant reminder that normalization, not excess, is therapeutic.
Shockwaves and Electricity: Harnessing Biophysical Modulation
Low-intensity shockwave therapy (Li-ESWT) has emerged as a non-invasive modality aimed at neovascularization and tissue regeneration. By inducing microtrauma, shockwaves stimulate angiogenesis, endothelial repair, and nerve regeneration. Clinical data suggest that combining daily tadalafil with Li-ESWT produces synergistic gains in erectile function compared to either therapy alone.
Similarly, vacuum erectile devices (VEDs) provide a mechanical means of augmenting cavernosal blood flow. While sometimes dismissed as cumbersome, when combined with PDE5 inhibitors, VEDs significantly amplified improvements in IIEF scores. In fact, one study reported gains as high as 8 points—one of the largest improvements across all adjuncts.
These methods remind us that restoring erectile function is not purely pharmacological; mechanical and regenerative cues can meaningfully recondition penile tissue.
Metabolic Modifiers: From Folic Acid to Metformin
ED is closely intertwined with systemic metabolic health. Endothelial dysfunction, insulin resistance, and oxidative stress all undermine penile hemodynamics. Recognizing this, researchers have tested metabolic adjuncts alongside PDE5 inhibitors.
- Folic acid supplementation improved erectile scores, likely through enhanced endothelial nitric oxide bioavailability.
- Metformin, a mainstay of type 2 diabetes treatment, not only reduced insulin resistance but also augmented response to tadalafil.
- ACE inhibitors appeared to confer additive vascular benefit, though data remain limited.
These findings align with the broader principle that managing ED effectively often requires addressing underlying cardiometabolic dysfunction. The penis, after all, is a barometer of vascular health.
Post-Prostatectomy Rehabilitation: A Special Population
Radical prostatectomy is notorious for leaving men with ED, even when nerve-sparing techniques are employed. Nerve injury, hypoxia-induced fibrosis, and endothelial dysfunction all conspire to undermine recovery. In this context, combination strategies hold particular promise.
Trials pairing PDE5 inhibitors with L-carnitine derivatives, antioxidants, or shockwave therapy have yielded improvements in erectile function during postoperative rehabilitation. The rationale is straightforward: protecting or regenerating penile tissue while maintaining cavernosal oxygenation maximizes the chance of functional recovery. Here, sildenafil is less about acute enhancement and more about long-term penile preservation.
Safety Considerations: More Is Not Necessarily More Dangerous
A common concern is that adding multiple agents could increase adverse events. Reassuringly, across 32 randomized trials, the incidence of treatment-related side effects did not differ significantly between combination therapy and monotherapy. Headache, flushing, dyspepsia, and nasal congestion remained the most common complaints, typically mild and self-limited.
Of course, clinicians must remain vigilant about drug–drug interactions, especially in men with polypharmacy. Yet the data suggest that combination therapy, when thoughtfully designed, enhances efficacy without sacrificing safety.
Clinical Implications: When to Consider Combination Therapy
The meta-analysis supports several practical take-home messages:
- Combination therapy is particularly valuable in PDE5 inhibitor nonresponders, hypogonadal men, diabetics, and post-prostatectomy patients.
- Strategies involving testosterone, shockwaves, or vacuum devices yield consistent and clinically meaningful improvements.
- Metabolic adjuncts such as folic acid and metformin may benefit patients with underlying vascular or diabetic disease.
- Safety profiles are comparable to monotherapy, making escalation feasible in most patients.
For clinicians, this translates into a more proactive approach: rather than abandoning PDE5 inhibitors after suboptimal response, consider what complementary therapy might unlock efficacy.
Conclusion: A Future of Personalised, Multimodal ED Therapy
The evolution of ED management mirrors the broader trend in medicine toward personalized, multimodal care. Sildenafil was a revolution, but not a final destination. The evidence now points toward combination strategies that tailor therapy to pathophysiology, patient preference, and systemic health.
In this vision, sildenafil and its PDE5 inhibitor counterparts remain foundational, but they are joined by testosterone, shockwaves, metabolic regulators, and mechanical devices. Together, they shift the paradigm from symptomatic relief to functional restoration. The future of ED therapy may well lie not in a single pill, but in an orchestra of synergistic interventions.
FAQ
1. Why does sildenafil fail in some men with erectile dysfunction?
Sildenafil relies on intact nitric oxide pathways. In men with severe diabetes, vascular disease, or nerve injury, these pathways may be impaired, reducing responsiveness.
2. Is combination therapy safe compared with monotherapy?
Yes. Large analyses show no significant increase in adverse events when PDE5 inhibitors are combined with testosterone, shockwaves, or other adjuncts.
3. Who benefits most from combination therapy?
Nonresponders to PDE5 inhibitors, men with hypogonadism, diabetics, and those recovering from prostatectomy derive the greatest benefit.
4. Should combination therapy replace sildenafil monotherapy as first-line treatment?
Not universally. Monotherapy remains appropriate for many men, but in difficult-to-treat or refractory cases, combination strategies should be considered early.